Romano–Ward syndrome
| Romano–Ward syndrome | |
|---|---|
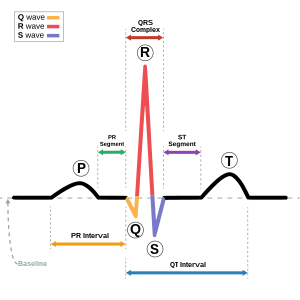 | |
| Schematic representation of normal ECG trace (sinus rhythm), with waves, segments, and intervals labeled. | |
| Causes | Mutations in the KCNQ1, KCNH2, and SCN5A genes [1] |
| Diagnostic method | EKG, Exercise test[2] |
| Treatment | Beta-adrenergic blockade [3] |
Romano–Ward syndrome is the most common subtype of Long QT syndrome, a genetic heart condition that affects the electrical properties of heart muscle cells. The condition makes those affected at risk of abnormal heart rhythms which can lead to fainting, seizures, or sudden death. [4][1][5]
Romano-Ward syndrome can be distinguished clinically from other forms of Long QT by affecting only the electrical properties of the heart, while other forms of long QT can also affect other parts of the body. The condition may be treated using medication such as beta-blockers, an implantable cardioverter-defibrillator, or surgery to disrupt the sympathetic nervous system. [6]
Contents
Signs and symptoms[edit]
Romano–Ward syndrome presents the following in an affected individual:[7]
- Ventricular fibrillation
- Syncope
- Torsade de pointes
- Abnormality of ear
Genetics[edit]
Romano–Ward syndrome is a descriptive term for a group of subtypes of long QT syndrome, specifically subtypes LQT1-6 and LQT9-16. [6] These subtypes are characterised by autosomal dominant inheritance and only affect the electrical activity of the heart. Other forms of Long QT include Jervell-Lange-Nielsen syndrome, characterised by autosomal recessive inheritance and congenital deafness,[6] Anderson-Tawil syndrome (LQT7) which combines a prolonged QT interval with periodic paralysis and an abnormally shaped face, [6]and Timothy syndrome (LQT8) which combines a prolonged QT interval, abnormalities in the structure of the heart, and autism-spectrum disorder. [6]
| Type | OMIM | Gene | Notes |
| LQT1 | 192500 | KCNQ1 | Encodes the α-subunit of the slow delayed rectifier potassium channel KV7.1 carrying the potassium current IKs. [8] |
| LQT2 | 152427 | KCNH2 | Also known as hERG. Encodes the α-subunit of the rapid delayed rectifier potassium channel KV11.1 carrying the potassium current IKr. [8] |
| LQT3 | 603830 | SCN5A | Encodes the e α-subunit of the cardiac sodium channel NaV1.5 carrying the sodium current INa. [8] |
| LQT4 | 600919 | ANK2 | Encodes Ankyrin B which anchors the ion channels in the cell. Disputed true association with QT prolongation. [8] |
| LQT5 | 176261 | KCNE1 | Encodes MinK, a potassium channel β-subunit. [8] |
| LQT6 | 603796 | KCNE2 | Encodes MiRP1, a potassium channel β-subunit. [8] |
| LQT9 | 611818 | CAV3 | Encodes Caveolin-3 responsible for forming membrane pouches known as caveolae. Mutations in this gene may increase the late sodium INa. [8] |
| LQT10 | 611819 | SCN4B | Encodes the β4-subunit of the cardiac sodium channel. [8] |
| LQT11 | 611820 | AKAP9 | Encode A-kinase associated protein which interacts with KV7.1. [8] |
| LQT12 | 601017 | SNTA1 | Encodes syntrophin-α1. Mutations in this gene may increase the late sodium current INa. [8] |
| LQT13 | 600734 | KCNJ5 | Also known as GIRK4, encodes G protein-sensitive inwardly rectifying potassium channels (Kir3.4) which carry the potassium current IK(ACh). [8] |
| LQT14 | 616247 | CALM1 | Encodes calmodulin-1, a calcium-binding messenger protein that interacts with the calcium current ICa(L). [8] |
| LQT15 | 616249 | CALM2 | Encodes calmodulin-2, a calcium-binding messenger protein that interacts with the calcium current ICa(L). [8] |
| LQT16 | 114183 | CALM3 | Encodes calmodulin-3, a calcium-binding messenger protein that interacts with the calcium current ICa(L). [8] |
Mechanism[edit]
In the Romano-Ward forms of Long QT syndrome, genetic mutations affect how positively-charged ions, such as potassium, sodium and calcium ions are transported in and out of heart cells. Many of these genes encode proteins which form or interact with ion channels. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in any of these genes alter the structure or function of channels, which changes the flow of ions between cells, a disruption in ion transport alters the way the heart beats, leading to abnormal heart rhythm characteristic of the syndrome.[3][9][10][11]
The protein made by the ANK2 gene ensures that other proteins, particularly ion channels, are inserted into the cell membrane appropriately. A mutation in the ANK2 gene likely alters the flow of ions between cells in the heart, which disrupts the heart's normal rhythm and results in the features of Romano–Ward syndrome.[medical citation needed]
Diagnosis[edit]
In terms of the diagnosis of Romano–Ward syndrome the following is done to ascertain the condition (the Schwartz Score helps in so doing):[2]
Treatment[edit]
Treatment for Romano–Ward syndrome can deal with the imbalance between the right and left sides of the sympathetic nervous system which may play a role in the cause of this syndrome. The imbalance can be temporarily abolished with a left stellate ganglion block, which shorten the QT interval. If this is successful, surgical ganglionectomy can be performed as a permanent treatment.[12]Ventricular dysrhythmia may be managed by beta-adrenergic blockade (propranolol)[13][3]
Epidemiology[edit]
Romano-Ward syndrome is the most common form of inherited long QT syndrome, affecting an estimated 1 in 7,000 people worldwide.[citation needed]
See also[edit]
References[edit]
- ^ a b Reference, Genetics Home. "Romano-Ward syndrome". Genetics Home Reference. Retrieved 2017-04-01.
- ^ a b Mizusawa, Yuka; Horie, Minoru; Wilde, Arthur AM (2014-01-01). "Genetic and Clinical Advances in Congenital Long QT Syndrome". Circulation Journal. 78 (12): 2827–2833. doi:10.1253/circj.CJ-14-0905.
- ^ a b c RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Romano Ward syndrome". www.orpha.net. Retrieved 2017-04-01.
- ^ "Long QT syndrome 1 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2018-04-17.
- ^ Alders, Mariëlle; Christiaans, Imke (1993-01-01). "Long QT Syndrome". In Pagon, Roberta A.; Adam, Margaret P.; Ardinger, Holly H.; Wallace, Stephanie E.; Amemiya, Anne; Bean, Lora JH; Bird, Thomas D.; Ledbetter, Nikki; Mefford, Heather C. GeneReviews(®). Seattle (WA): University of Washington, Seattle. PMID 20301308.update 2015
- ^ a b c d e "2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death". Europace: euv319. 29 August 2015. doi:10.1093/europace/euv319. ISSN 1099-5129. Retrieved 28 October 2018.
- ^ "Long QT syndrome 1 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2017-04-01.
- ^ a b c d e f g h i j k l m n Giudicessi, John R.; Wilde, Arthur A. M.; Ackerman, Michael J. (October 2018). "The genetic architecture of long QT syndrome: A critical reappraisal". Trends in Cardiovascular Medicine. 28 (7): 453–464. doi:10.1016/j.tcm.2018.03.003. ISSN 1873-2615. PMID 29661707.
- ^ "ANK2 ankyrin 2 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2017-04-06.
- ^ "KCNE1 potassium voltage-gated channel subfamily E regulatory subunit 1 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2017-04-06.
- ^ "KCNE2 potassium voltage-gated channel subfamily E regulatory subunit 2 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2017-04-06.
- ^ Hines, Roberta, Soeltin's Anesthesia and Co-existing Disease (4 ed.), Elsevir, p. 89
- ^ "OMIM Entry - # 192500 - LONG QT SYNDROME 1; LQT1". omim.org. Retrieved 1 April 2017.
Further reading[edit]
- Kelly, Evelyn B. (2013-01-07). Encyclopedia of Human Genetics and Disease. ABC-CLIO. ISBN 9780313387135. retrieved 2017-04-07
- Nakano, Yukiko; Shimizu, Wataru (2016-01-01). "Genetics of long-QT syndrome". Journal of Human Genetics. 61 (1): 51–55. doi:10.1038/jhg.2015.74. ISSN 1434-5161. PMID 26108145.
External links[edit]
| Classification | |
|---|---|
| External resources |

