Back pain
| Back pain | |
|---|---|
 | |
| Different regions (curvatures) of the vertebral column | |
| Specialty | Orthopedics |
Back pain is pain felt in the back. The back is divided into middle back pain (thoracic), lower back pain (lumbar) or coccydynia (tailbone or sacral pain) based on the segment affected.[1] Neck pain (cervical), which is considered an independent entity, can involve similar processes. The lumbar area is the most common area for pain, as it supports most of the weight in the upper body.[2] Episodes of back pain may be acute, sub-acute, or chronic depending on the duration. The pain may be characterized as a dull ache, shooting or piercing pain, or a burning sensation. Discomfort can radiate into the arms and hands as well as the legs or feet,[3] and may include numbness,[1] or weakness in the legs and arms.
The majority of back pain seen in primary care is nonspecific with no identifiable causes.[4][5] Common identifiable causes of back pain include degenerative or traumatic changes to the discs and facets joints, which can then cause secondary pain in the muscles, and nerves, and referred pain to the bones, joints and extremities.[3] Diseases and inflammation of the gallbladder, pancreas, aorta, and kidneys may also cause referred pain in the back.[3] Tumors of the verteba, neural tissues and adjacent structures can also manifest as back pain.
Back pain is common, with about nine out of ten adults experiencing it at some point in their life, and five out of ten working adults having it every year.[6] Some estimate up to 95% of Americans will experience back pain at some point in their lifetime.[2] It is the most common cause of chronic pain, and is a major contributor of missed work and disability.[2] For most individuals, back pain is self-limited. In most cases of herniated disks and stenosis, rest, injections or surgery have similar general pain resolution outcomes on average after one year. In the United States, acute low back pain is the fifth most common reason for physician visits and causes 40% of missed days off work.[7] Additionally, it is the single leading cause of disability worldwide.[8]
Contents
Classification[edit]
Back pain is classified in terms of duration of symptoms.[9]
- Acute back pain lasts <6 weeks
- Subacute back pain lasts between 6 to 12 weeks.
- Chronic back pain lasts for greater than 12 weeks.
Causes[edit]
There are many causes of back pain, including blood vessels, internal organs, infections, mechanical, and autoimmune causes.[10] Approximately 90 percent of people with back pain are diagnosed with nonspecific acute back pain in which there is no serious underlying pathology.[11] In approximately 10 percent of people, cause can be identified through diagnostic imaging.[11] Less than 2 percent are attributed to secondary factors, with metastatic cancers and serious infections, such as spinal osteomyelitis and epidural abscesses, accounting for around 1 percent.[12]
| Cause | % of patients with back pain |
|---|---|
| Nonspecific | 90%[7] |
| Vertebral compression fracture | 4%[13] |
| Metastatic cancer | 0.7%[7] |
| Infection | 0.01%[7] |
| Cauda equina | 0.04%[14] |
Nonspecific back pain[edit]
In as many as 90 percent of cases, no physiological causes or abnormalities on diagnostic tests can be found.[15] Nonspecific back pain can be due to back strain/sprain. The cause is peripheral injury to muscle or ligaments. The patient may or may not recall the cause.[9] The pain can present acutely but in some cases can persist, leading to chronic pain.
Chronic back pain in people with otherwise normal scans can result from central sensitization, where an initial injury causes a longer-lasting state of heightened sensitivity to pain. This persistent state maintains pain even after the initial injury has healed.[16] Treatment of sensitization may involve low doses of anti-depressants and directed rehabilitation such as physical therapy.[17]
Structural causes of back pain[edit]
Spinal disk disease[edit]
Spinal disk disease occurs when the nucleus pulposus, a gel-like material in the inner core of the vertebral disc, ruptures.[18] Rupturing of the nucleus pulposus can lead to compression of nerve roots. Symptoms may be unilateral or bilateral, and correlate to the region of the spine affected. The most common region for spinal disk disease is at L4-L5 or L5-S1. The risk for lumbar disc disease is increased in overweight individuals due to the increased compressive force on the nucleus pulposus.[18]
Severe spinal cord compression is considered a surgical emergency and requires decompression to preserve motor and sensory function. Cauda equina syndrome refers to severe compression of the cauda equina and presents initially with pain followed by motor and sensory.[14] Bladder incontinence is seen in later stages of the cauda equina syndrome.
Degenerative spine disease[edit]
Spondylosis, or degenerative arthritis of the spine, occurs when the intervertebral disc undergoes degenerative changes, causing the disc to fail at cushioning the vertebrae. There is an association between intervertebral disc space narrowing and lumbar spine pain.[19] The space between the vertebrae becomes more narrow, resulting in compression and irritation of the nerves.[20]
Spondylolithesis is the anterior shift of one vertebra compared to the neighboring vertebra. It is associated with age-related degenerative changes as well as trauma and congenital anomalies.
Spinal stenosis can occur in cases of severe spondylosis, spondylotheisis and age associated thickening of the ligamentum flavum. Spinal stenosis involves narrowing of the spinal canal and typically presents in patients greater than 60 years of age. Neurogenic claudication can occur in cases of severe lumbar spinal stenosis and presents with syptoms of pain in the lower back, buttock or leg that is worsened by standing and relieved by sitting.
Vertebral compression fractures occurs in 4 percent of patients presenting to primary care with low back pain.[21] Risk factors include age, female gender, history of osteoporosis, and chronic glucocorticoid use. Fractures can occur due to trauma but in many cases can be asymptomatic.
Systemic causes of back pain[edit]
Infection[edit]
Common infectious causes of back pain include osteomyelitis, septic diskitis, paraspinal abcess, and epidural abscess.[18] Infectious causes that lead to back pain involve various structures surrounding the spine.
Osteomyelitis is the bacterial infection of the bone. Vertebral osteomyelitis is most commonly caused by staphyloccocci.[18] Risk factors include skin infection, urinary tract infection, IV catheter use, IV drug use, previous endocarditis, and lung disease.
Spinal epidural abscess is also commonly caused by severe infection with bacteremia. Risk factors include recent epidural, IV drug use, or recent infection.
Neoplasms[edit]
Spread of cancer to the bone or spinal cord can lead to back pain. Bone is one of the most common sites of metastatic lesions. Patients typically have a history of malignancy. Common types of cancer that present with back pain include multiple myeloma, lymphoma, leukemia, spinal cord tumors, primary vertebral tumors, and prostate cancer.[13] Back pain is present in 29% of patients with systemic cancer.[18] Unlike other causes of back pain which common affect the lumbar spine, the thoracic spine is most commonly affected.[18] The pain can be associated with systemic symptoms such as weight loss, chills, fever, nausea and vomiting.[18] Unlike other causes of back pain, neoplasm-associated back pain is constant, dull, poorly localized, and worst with rest. Metasis to the bone also increases the risk of spinal cord compression or vertebral fractures which requires emergent surgical treatment.
Autoimmune[edit]
Inflammatory athritides such as ankylosing spondylitis, psoriatic arthritis, rheumatoid arthritis, and systemic lupus erythematosis can all cause varying levels of joint destruction. Among the inflammatory arhrithidies, ankylosing spondylitis is most closely associated with back pain due to the inflammatory distruction of the bony components of the spine. Ankylosing spondylitis is common in young men and presents with a range of possible symptoms such as uveitis, psoriasis, and inflammatory bowel disease.
Referred pain[edit]
Back pain can also be due to referred pain from another source. Referred pain occurs when pain is felt at a location different from the source of the pain. Disease processes that can present with back pain include pancreatitis, kidney stones, severe urinary tract infections, and abdominal aortic aneurysms.[9]
Risk factors[edit]
Obesity, sedentary lifestyle, and lack of exercise can increase a person's risk of back pain.[2] People who smoke are more likely to experience back pain than others.[22] Poor posture and weight gain in pregnancy are also risk factors for back pain. In general, fatigue can worsen pain.[2]
A few studies suggest that psychosocial factors such as on-the-job stress and dysfunctional family relationships may correlate more closely with back pain than structural abnormalities revealed in X-rays and other medical imaging scans.[23][24][25][26]
Diagnosis[edit]

Initial assessment of back pain consists of a history and physical examination.[28] Important characterizing features of the back pain include location, duration, severity, history of prior back pain, and possible trauma. Other important components of the patient history include age, physical trauma, prior history of cancer, fever, weight loss, urinary incontinence, progressive weakness, or expanding sensory changes, which can elicit red flags indicating a medical urgent condition.[28]
Physical examination of the back should assess for posture and deformities. Pain elicited by palpating certain structures may be helpful in localizing the affected area. A neurologic exam is needed to assess for changes in gait, sensation, and motor function.
Determining if there is radicular symptoms, such as pain, numbness, or weakness that radiates down limbs, is important for differentiating between central and peripheral causes of back pain. The straight leg test is a maneuver used to determine the presence of lumbosacral radiculopathy. Radiculopathy occurs when there is irritation in the nerve root, causing neurologic symptoms, such as numbness and tingling. Non-radicular back pain is most commonly caused by injury to the spinal muscles or ligaments, degenerative spinal disease, or a herniated disk.[10] Disk herniation and foraminal stenosis are the most common causes of radiculopathy.[10]
Imaging of the spine and laboratory tests is not recommended during the acute phase.[18] This assumes that there is no reason to expect that the person has an underlying problem.[29][18] In most cases, the pain goes away naturally after a few weeks.[29] Typically, people who do seek diagnosis through imaging are not likely to have a better outcome than those who wait for the condition to resolve.[29]
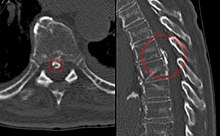
Imaging[edit]
Magnetic resonance imaging is the preferred modality for the evaluation of back pain and visualize bone, soft tissue, nerves, and ligaments. X-rays are a less costly initial option offered to patients with a low clinical suspicion of infection or malignancy and is combined with laboratory studies for interpretation.
Imaging is not needed in the majority of individuals with back pain. In cases of acute back pain, MRI is recommended for individuals with major risk factors/clinical suspicion for cancer, spinal infection, or severe progressive neurological deficits.[30] For patients with subacute to chronic back pain, MRI is recommended if there are minor risk factors for cancer, risk factors for ankylosing spondylitis, risk factors for vertebral compression fracture, significant trauma, or symptomatic spinal stenosis.[30]
Early imaging studies during the acute phase do not improve care or prognosis in patients.[31] Imaging findings are not correlated with severity or outcome.[32]
Laboratory studies[edit]
Laboratory studies are used to if there are suspicions for autoimmune causes, infection, or malignancy.[33][34] Laboratory testing may include white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).[10]
- Elevated ESR could indicate infection, malignancy, chronic disease, inflammation, trauma, or tissue ischemia.[10]
- Elevated CRP levels are associated with infection.[10]
Red flags[edit]
Imaging is not typically needed in the initial diagnosis or treatment of back pain. However, if there are certain "red flag" symptoms present plain radiographs (x-ray), CT scan, or magnetic resonance imaging (MRI) may be recommended. These red flags include:[35][10]
- History of cancer
- Unexplained weight loss
- Immunosuppression
- Urinary infection
- Intravenous drug use
- Prolonged use of corticosteroids
- Back pain not improved with conservative management
- History of significant trauma
- Minor fall or heavy lift in a potentially osteoporotic or elderly individual
- Acute onset of urinary retention, overflow incontinence, loss of anal sphincter tone, or fecal incontinence
- Saddle anesthesia
- Global or progressive motor weakness in the lower limbs
Prevention[edit]
There is moderate quality evidence that suggests the combination of education and exercise may reduce an individual's risk of developing an episode of low back pain.[36] Lesser quality evidence points to exercise alone as a possible deterrent to the risk of the onset of this condition.[36]
Management[edit]
Treatment of nonspecific back pain[edit]
Patients with uncomplicated back pain should be encouraged to remain active and return to normal activities.
The management goals when treating back pain are to achieve maximal reduction in pain intensity as rapidly as possible, to restore the individual's ability to function in everyday activities, to help the patient cope with residual pain, to assess for side-effects of therapy, and to facilitate the patient's passage through the legal and socioeconomic impediments to recovery. For many, the goal is to keep the pain to a manageable level to progress with rehabilitation, which then can lead to long-term pain relief. Also, for some people the goal is to use non-surgical therapies to manage the pain and avoid major surgery, while for others surgery may be the quickest way to feel better.[37]
Not all treatments work for all conditions or for all individuals with the same condition, and many find that they need to try several treatment options to determine what works best for them. The present stage of the condition (acute or chronic) is also a determining factor in the choice of treatment. Only a minority of people with back pain (most estimates are 1% - 10%) require surgery.[citation needed]
Non medical[edit]
Back pain is generally treated with non-pharmacological therapy first, as it typically resolves without the use of medication. Superficial heat and massage, acupuncture, and spinal manipulation therapy may be recommended.[38]
- Heat therapy is useful for back spasms or other conditions. A review concluded that heat therapy can reduce symptoms of acute and sub-acute low-back pain.[39]
- Regular activity and gentle stretching exercises is encouraged in uncomplicated back pain, and is associated with better long-term outcomes.[10][40] Physical therapy to strengthen the muscles in the abdomen and around the spine may also be recommended.[41] These exercises are associated with better patient satisfaction, although it has not been shown to provide functional improvement.[10] However, one study found that exercise is effective for chronic back pain, but not for acute pain.[citation needed] If used, they should be performed under supervision of a licensed health professional.[42]
- Massage therapy may give short-term pain relief, but not functional improvement, for those with acute lower back pain.[43] It may also give short-term pain relief and functional improvement for those with long-term (chronic) and sub-acute lower pack pain, but this benefit does not appear to be sustained after 6 months of treatment.[43] There does not appear to be any serious adverse effects associated with massage.[43]
- Acupuncture may provide some relief for back pain. However, further research with stronger evidence needs to be done.[44]
- Spinal manipulation is a widely-used method of treating back pain.[45] Immediate benefits can be significant, but long-term benefits can be variable.[41]
- "Back school" is an intervention that consists of both education and physical exercises.[46][47] There is no strong evidence supporting the use of Back School for treating acute, sub-acute, or chronic non-specific back pain.[46][47]
Medication[edit]
If non-pharmacological measures are not effective, medications may be tried.
- Non-steroidal anti-inflammatory drugs (NSAIDs) are typically tried first.[38] NSAIDs have been shown to be more effective than placebo, and are usually more effective than paracetamol (acetaminophen).[48]
- Long-term use of opioids has not been tested in order to determine if it is effective or safe for treating chronic lower back pain.[49][50] For severe back pain not relieved by NSAIDs or acetaminophen, opioids may be used.[citation needed] Opioids may not be better than NSAIDs or antidepressants for chronic back pain with regards to pain relief and gain of function.[50]
- Skeletal muscle relaxers may also be used.[38] Their short term use has been shown to be effective in the relief of acute back pain.[51] However, the evidence of this effect has been disputed, and these medications do have negative side-effects.[49]
- In people with nerve root pain and acute radiculopathy, there is evidence that a single dose of steroids, such as dexamethasone, may provide pain relief.[10]
- Epidural corticosteroid injection (ESI) is a procedure in which steroid medications are injected into the epidural space. The steroid medications reduce inflammation and thus decrease pain and improve function.[52] ESI has long been used to both diagnose and treat back pain, although recent studies have shown a lack of efficacy in treating low back pain.[53]
Indications for surgery[edit]
Surgery for back pain is typically used as a last resort, when serious neurological deficit is evident.[41] A 2009 systematic review of back surgery studies found that, for certain diagnoses, surgery is moderately better than other common treatments, but the benefits of surgery often decline in the long term.[54]
Surgery may sometimes be appropriate for people with severe myelopathy or cauda equina syndrome.[41] Causes of neurological deficits can include spinal disc herniation, spinal stenosis, degenerative disc disease, tumor, infection, and spinal hematomas, all of which can impinge on the nerve roots around the spinal cord.[41] There are multiple surgical options to treat back pain, and these options vary depending on the cause of the pain.
When a herniated disc is compressing the nerve roots, hemi- or partial- laminectomy or discectomy may be performed, in which the material compressing on the nerve is removed.[41] A mutli-level laminectomy can be done to widen the spinal canal in the case of spinal stenosis. A foraminotomy or foraminectomy may also be necessary, if the vertebrae are causing significant nerve root compression.[41] A discectomy is performed when the intervertebral disc has herniated or torn. It involves removing the protruding disc, either a portion of it or all of it, that is placing pressure on the nerve root.[55] Total disc replacement can also be performed, in which the source of the pain (the damaged disc) is removed and replaced, while maintaining spinal mobility.[56] When an entire disc is removed (as in discectomy), or when the vertebrae are unstable, spinal fusion surgery may be performed. Spinal fusion is a procedure in which bone grafts and metal hardware is used to fix together two or more vertebrae, thus preventing the bones of the spinal column from compressing on the spinal cord or nerve roots.[57]
If infection, such as a spinal epidural abscess, is the source of the back pain, surgery may be indicated when a trial of antibiotics is ineffective.[41] Surgical evacuation of spinal hematoma can also be attempted, if the blood products fail to break down on their own.[41]
Pregnancy[edit]
About 50% of women experience low back pain during pregnancy.[58] Some studies have suggested women who have experienced back pain before pregnancy are at a higher risk of having back pain during pregnancy.[59] It may be severe enough to cause significant pain and disability in up to a third of pregnant women.[60][61] Back pain typically begins at around 18 weeks gestation, and peaks between 24 and 36 weeks gestation.[61] Approximately 16% of women who experienced back pain during pregnancy report continued back pain years after pregnancy, indicating those with significant back pain are at greater risk of back pain following pregnancy.[60][61]
Biomechanical factors of pregnancy shown to be associated with back pain include increased curvature of the lower back, or lumbar lordosis, to support the added weight on the abdomen.[61] Also, a hormone called relaxin is released during pregnancy that softens the structural tissues in the pelvis and lower back to prepare for vaginal delivery. This softening and increased flexibility of the ligaments and joints in the lower back can result in pain.[61] Back pain in pregnancy is often accompanied by radicular symptoms, suggested to be caused by the fetus pressing on the sacral plexus and lumbar plexus in the pelvis.[61][59]
Typical factors aggravating the back pain of pregnancy include standing, sitting, forward bending, lifting, and walking. Back pain in pregnancy may also be characterized by pain radiating into the thigh and buttocks, night-time pain severe enough to wake the patient, pain that is increased during the night-time, or pain that is increased during the day-time.[60]
Local heat, acetaminophen (paracetamol), and massage can be used to help relieve the pain. Avoiding standing for prolonged periods of time is also suggested.[62]
Economics[edit]
Although back pain does not typically cause permanent disability, it is a significant contributor to physician visits and missed work days in the United States, and is the single leading cause of disability worldwide.[7][8] The American Academy of Orthopaedic Surgeons report approximately 12 million visits to doctor's offices each year are due to back pain.[2] Missed work and disability related to low back pain costs over $50 billion each year in the United States.[2] In the United Kingdom in 1998, approximately £1.6 billion per year was spent on expenses related to disability from back pain.[2]
References[edit]
- ^ a b "Paresthesia Definition and Origin". dictionary.com. Retrieved 1 August 2015.
- ^ a b c d e f g h Church E, Odle T. Diagnosis and treatment of back pain. Radiologic Technology [serial online]. November 2007;79(2):126-204. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed December 12, 2017.
- ^ a b c Burke GL (2008). "Chapter 3: The Anatomy of Pain in Backache". Backache:From Occiput to Coccyx. Vancouver, BC: MacDonald Publishing. ISBN 978-0-920406-47-2.
- ^ Deyo, Richard A.; Weinstein, James N. (2001-02-01). "Low Back Pain". New England Journal of Medicine. 344 (5): 363–370. doi:10.1056/NEJM200102013440508. ISSN 0028-4793. PMID 11172169.
- ^ Cohen, Steven P. (February 2015). "Epidemiology, diagnosis, and treatment of neck pain". Mayo Clinic Proceedings. 90 (2): 284–299. doi:10.1016/j.mayocp.2014.09.008. ISSN 1942-5546. PMID 25659245.
- ^ A.T. Patel, A.A. Ogle. "Diagnosis and Management of Acute Low Back Pain". American Academy of Family Physicians. Retrieved March 12, 2007.
- ^ a b c d e Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA (Jul–Aug 2009). "Comprehensive review of epidemiology, scope, and impact of spinal pain". Pain Physician. 12 (4): E35–70. PMID 19668291.
- ^ a b Institute for Health Metrics and Evaluation. "2010 Global Burden of Disease Study"
- ^ a b c Chou, Roger; Qaseem, Amir; Snow, Vincenza; Casey, Donald; Cross, J. Thomas; Shekelle, Paul; Owens, Douglas K.; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians (2007-10-02). "Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society". Annals of Internal Medicine. 147 (7): 478–491. ISSN 1539-3704. PMID 17909209.
- ^ a b c d e f g h i j Walls, Ron M.; Hockberger, Robert S.; Gausche-Hill, Marianne (2017-05-18). Rosen's emergency medicine : concepts and clinical practice. Walls, Ron M.,, Hockberger, Robert S.,, Gausche-Hill, Marianne (Ninth ed.). Philadelphia, PA. ISBN 9780323354790. OCLC 989157341.
- ^ a b Slipman, Curtis W.; et al., eds. (2008). Interventional spine : an algorithmic approach. Philadelphia, PA: Saunders Elsevier. p. 13. ISBN 978-0-7216-2872-1.
- ^ "Back Pain". Archived from the original on May 6, 2011. Retrieved April 30, 2018.
- ^ a b author., Stern, Scott D. C. (2014-10-28). Symptom to diagnosis : an evidence-based guide. ISBN 9780071803441. OCLC 894996548.
- ^ a b Orendácová, J.; Cízková, D.; Kafka, J.; Lukácová, N.; Marsala, M.; Sulla, I.; Marsala, J.; Katsube, N. (August 2001). "Cauda equina syndrome". Progress in Neurobiology. 64 (6): 613–637. ISSN 0301-0082. PMID 11311464.
- ^ van den Bosch MA, Hollingworth W, Kinmonth AL, Dixon AK (January 2004). "Evidence against the use of lumbar spine radiography for low back pain". Clinical Radiology. 59 (1): 69–76. doi:10.1016/j.crad.2003.08.012. PMID 14697378.
- ^ Woolf, Clifford J (2011-03-01). "Central sensitization: Implications for the diagnosis and treatment of pain". Pain. 152 (3 Suppl): S2–15. doi:10.1016/j.pain.2010.09.030. ISSN 0304-3959. PMC 3268359. PMID 20961685.
- ^ Verdu, Bénédicte; Decosterd, Isabelle; Buclin, Thierry; Stiefel, Friedrich; Berney, Alexandre (2008-01-01). "Antidepressants for the treatment of chronic pain". Drugs. 68 (18): 2611–2632. doi:10.2165/0003495-200868180-00007. ISSN 0012-6667. PMID 19093703.
- ^ a b c d e f g h i HerausgeberIn., Jameson, J. Larry (2018-08-13). Harrison's principles of internal medicine. ISBN 9781259644030. OCLC 1041928452.
- ^ Raastad, Joachim (2015). "The association between lumbar spine radiographic features and low back pain: A systematic review and meta-analysis". Seminars in Arthritis and Rheumatism. 44 (5): 571–585. doi:10.1016/j.semarthrit.2014.10.006. PMID 25684125.
- ^ Lavelle, W. F., Kitab, S. A., Ramakrishnan, R., & Benzel, E. C. (2017). Anatomy of Nerve Root Compression, Nerve Root Tethering, and Spinal Instability. In Benzel's Spine Surgery (4th ed., pp. 200-205). Philadelphia, PA: Elsevier. ISBN 978-0-323-40030-5
- ^ Jarvik, Jeffrey G.; Deyo, Richard A. (2002-10-01). "Diagnostic evaluation of low back pain with emphasis on imaging". Annals of Internal Medicine. 137 (7): 586–597. ISSN 1539-3704. PMID 12353946.
- ^ Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E (January 2010). "The association between smoking and low back pain: a meta-analysis". The American Journal of Medicine. 123 (1): 87.e7–35. doi:10.1016/j.amjmed.2009.05.028. PMID 20102998.
- ^ Burton AK, Tillotson KM, Main CJ, Hollis S (March 1995). "Psychosocial predictors of outcome in acute and subchronic low back trouble". Spine. 20 (6): 722–8. doi:10.1097/00007632-199503150-00014. PMID 7604349.
- ^ Carragee EJ, Alamin TF, Miller JL, Carragee JM (2005). "Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain". The Spine Journal. 5 (1): 24–35. doi:10.1016/j.spinee.2004.05.250. PMID 15653082.
- ^ Hurwitz EL, Morgenstern H, Yu F (May 2003). "Cross-sectional and longitudinal associations of low-back pain and related disability with psychological distress among patients enrolled in the UCLA Low-Back Pain Study". Journal of Clinical Epidemiology. 56 (5): 463–71. doi:10.1016/S0895-4356(03)00010-6. PMID 12812821.
- ^ Dionne CE (July 2005). "Psychological distress confirmed as predictor of long-term back-related functional limitations in primary care settings". Journal of Clinical Epidemiology. 58 (7): 714–8. doi:10.1016/j.jclinepi.2004.12.005. PMID 15939223.
- ^ Thiruganasambandamoorthy, Venkatesh; Turko, Ekaterina; Ansell, Dominique; Vaidyanathan, Aparna; Wells, George A.; Stiell, Ian G. (2014-7). "Risk factors for serious underlying pathology in adult emergency department nontraumatic low back pain patients". The Journal of Emergency Medicine. 47 (1): 1–11. doi:10.1016/j.jemermed.2013.08.140. ISSN 0736-4679. PMID 24725822. Check date values in:
|date=(help) - ^ a b editor., Usatine, Richard, editor. Smith, Mindy A., editor. Mayeaux, E. J., Jr., editor. Chumley, Heidi S. (2019-01-07). The color atlas and synopsis of family medicine. ISBN 9781259862052. OCLC 1080576440.CS1 maint: Extra text: authors list (link)
- ^ a b c *Consumer Reports; American College of Physicians; Annals of Internal Medicine (April 2012), "Imaging tests for lower-back pain: Why you probably don't need them." (PDF), High Value Care, Consumer Reports, retrieved 23 December 2013
- American College of Physicians (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Physicians, retrieved 10 December 2013
- National Collaborating Centre for Primary Care (May 2009), Low back pain: early management of persistent non-specific low back pain, National Institute for Health and Clinical Excellence, retrieved 9 September 2012
- National Collaborating Centre for Primary Care (13 January 2011), "ACR Appropriateness Criteria low back pain", Agency for Healthcare Research and Quality, American College of Radiology, archived from the original on 16 September 2012, retrieved 9 September 2012
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, Owens DK (October 2007). "Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society". Annals of Internal Medicine. 147 (7): 478–91. doi:10.7326/0003-4819-147-7-200710020-00006. PMID 17909209.
- "Low Back Pain". Occupational medicine practice guidelines : evaluation and management of common health. [S.l.]: Acoem. 2011. ISBN 978-0-615-45228-9.
- ^ a b Chou, Roger; Qaseem, Amir; Owens, Douglas K.; Shekelle, Paul; Clinical Guidelines Committee of the American College of Physicians (2011-02-01). "Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians". Annals of Internal Medicine. 154 (3): 181–189. CiteSeerX 10.1.1.690.1604. doi:10.7326/0003-4819-154-3-201102010-00008. ISSN 1539-3704. PMID 21282698.
- ^ Chou, Roger; Fu, Rongwei; Carrino, John A.; Deyo, Richard A. (2009-02-07). "Imaging strategies for low-back pain: systematic review and meta-analysis". Lancet. 373 (9662): 463–472. doi:10.1016/S0140-6736(09)60172-0. ISSN 1474-547X. PMID 19200918.
- ^ Oland, G.; Hoff, T. G. (1996-09-01). "Intraspinal cross-section areas measured on myelography--computed tomography. The relation to outcome in nonoperated lumbar disc herniation". Spine. 21 (17): 1985–1989, discussion 1990. ISSN 0362-2436. PMID 8883199.
- ^ Kapeller, P.; Fazekas, F.; Krametter, D.; Koch, M.; Roob, G.; Schmidt, R.; Offenbacher, H. (1997). "Pyogenic infectious spondylitis: clinical, laboratory and MRI features". European Neurology. 38 (2): 94–98. doi:10.1159/000113167. ISSN 0014-3022. PMID 9286631.
- ^ Deyo, R. A.; Diehl, A. K. (May 1988). "Cancer as a cause of back pain: frequency, clinical presentation, and diagnostic strategies". Journal of General Internal Medicine. 3 (3): 230–238. ISSN 0884-8734. PMID 2967893.
- ^ Patel ND, Broderick DF, Burns J, et al. ACR Appropriateness Criteria Low Back Pain. Available at https://acsearch.acr.org/docs/69483/Narrative/. American College of Radiology. Accessed Dec 12, 2017.
- ^ a b Steffens D, Maher CG, Pereira LS, Stevens ML, Oliveira VC, Chapple M, Teixeira-Salmela LF, Hancock MJ (January 2016). "Prevention of Low Back Pain: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 176 (2): 199–208. doi:10.1001/jamainternmed.2015.7431. PMID 26752509.
- ^ Baron, R; Binder, A; Attal, N; Casale, R; Dickenson, AH; Treede, RD (July 2016). "Neuropathic low back pain in clinical practice". European Journal of Pain. 20 (6): 861–73. doi:10.1002/ejp.838. PMC 5069616. PMID 26935254.
- ^ a b c Stockwell, Serena (2017-05-01). "New Clinical Guideline for Low Back Pain Says Try Nondrug Therapies First". American Journal of Nursing. 117 (5): 16. doi:10.1097/01.naj.0000516263.01592.38. ISSN 0002-936X. PMID 28448354.
- ^ French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ (April 2006). "A Cochrane review of superficial heat or cold for low back pain". Spine. 31 (9): 998–1006. doi:10.1097/01.brs.0000214881.10814.64. PMID 16641776.
- ^ Dahm, Kristin Thuve; Brurberg, Kjetil G.; Jamtvedt, Gro; Hagen, Kåre Birger (2010-06-16). "Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica". The Cochrane Database of Systematic Reviews (6): CD007612. doi:10.1002/14651858.CD007612.pub2. ISSN 1469-493X. PMID 20556780.
- ^ a b c d e f g h i Wall and Melzack's textbook of pain. McMahon, S. B. (Stephen B.) (6th ed.). Philadelphia, PA: Elsevier/Saunders. 2013. ISBN 9780702040597. OCLC 841325533.
- ^ Hayden JA, van Tulder MW, Malmivaara A, Koes BW (2005). "Exercise therapy for treatment of non-specific low back pain". The Cochrane Database of Systematic Reviews (3): CD000335. doi:10.1002/14651858.CD000335.pub2. PMID 16034851.
- ^ a b c Furlan, Andrea D.; Giraldo, Mario; Baskwill, Amanda; Irvin, Emma; Imamura, Marta (2015-09-01). "Massage for low-back pain". The Cochrane Database of Systematic Reviews (9): CD001929. doi:10.1002/14651858.CD001929.pub3. ISSN 1469-493X. PMID 26329399.
- ^ Yeganeh, Mohsen (May 1, 2017). "The effectiveness of acupuncture, acupressure and chiropractic interventions on treatment of chronic nonspecific low back pain in Iran: A systematic review and meta-analysis". Complementary Therapies in Clinical Practice. 27: 11–18. doi:10.1016/j.ctcp.2016.11.012. PMID 28438274 – via ClinicalKey.
- ^ Burke GL (2008). "Chapter 8: The Techniques of Traction and Manipulation of the Spine". Backache:From Occiput to Coccyx. Vancouver, BC: MacDonald Publishing. ISBN 978-0-920406-47-2.
- ^ a b Poquet, N; Lin, CW; Heymans, MW; van Tulder, MW; Esmail, R; Koes, BW; Maher, CG (26 April 2016). "Back schools for acute and subacute non-specific low-back pain". The Cochrane Database of Systematic Reviews. 4: CD008325. doi:10.1002/14651858.CD008325.pub2. PMID 27113258.
- ^ a b Parreira, Patrícia; Heymans, Martijn W.; van Tulder, Maurits W.; Esmail, Rosmin; Koes, Bart W.; Poquet, Nolwenn; Lin, Chung-Wei Christine; Maher, Christopher G. (2017). "Back Schools for chronic non-specific low back pain". The Cochrane Database of Systematic Reviews. 8: CD011674. doi:10.1002/14651858.CD011674.pub2. ISSN 1469-493X. PMID 28770974.
- ^ Staal JB, de Bie R, de Vet HC, Hildebrandt J, Nelemans P (2008). "Injection therapy for subacute and chronic low-back pain". The Cochrane Database of Systematic Reviews (3): CD001824. doi:10.1002/14651858.CD001824.pub3. PMID 18646078.
- ^ a b Sudhir, Amita; Perina, Debra (2018). "Musculoskeletal Back Pain". Rosen's Emergency Medicine: Concepts and Clinical Practice. Elsevier. pp. 569–576. ISBN 9780323354790 – via ClinicalKey.
- ^ a b Chaparro, LE; Furlan, AD; Deshpande, A; Mailis-Gagnon, A; Atlas, S; Turk, DC (27 August 2013). "Opioids compared to placebo or other treatments for chronic low-back pain". The Cochrane Database of Systematic Reviews (8): CD004959. doi:10.1002/14651858.CD004959.pub4. PMID 23983011.
- ^ van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM (2003). "Muscle relaxants for non-specific low back pain". The Cochrane Database of Systematic Reviews (2): CD004252. doi:10.1002/14651858.CD004252. PMID 12804507.
- ^ Terry Canale, S.; Azar, Frederick M.; Beaty, James H. (2016-11-21). Campbell's operative orthopaedics. Azar, Frederick M.,, Canale, S. T. (S. Terry),, Beaty, James H.,, Preceded by: Campbell, Willis C. (Willis Cohoon), 1880-1941. (Thirteenth ed.). Philadelphia, PA. ISBN 9780323374620. OCLC 962333989.
- ^ Jankovic, Joseph; Daroff, Robert B.; Mazziotta, John C.; Pomeroy, Scott Loren (2015-11-23). Bradley's neurology in clinical practice. Daroff, Robert B.,, Jankovic, Joseph,, Mazziotta, John C.,, Pomeroy, Scott Loren,, Bradley, W. G. (Walter George) (Seventh ed.). London. ISBN 9780323287838. OCLC 932031625.
- ^ Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD (May 2009). "Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline". Spine. 34 (10): 1094–109. doi:10.1097/BRS.0b013e3181a105fc. PMID 19363455.
- ^ "Surgery For Back Pain". Retrieved June 18, 2010.
- ^ Benzel, Edward C.; Steinmetz, Michael P. (2016-09-02). Benzel's spine surgery : techniques, complication avoidance, and management. Steinmetz, Michael P.,, Benzel, Edward C. (Fourth ed.). Saint Louis. ISBN 9780323400305. OCLC 953660061.
- ^ Burke, G.L., "Backache from Occiput to Coccyx" Chapter 9
- ^ Ostgaard HC, Andersson GB, Karlsson K (May 1991). "Prevalence of back pain in pregnancy". Spine. 16 (5): 549–52. doi:10.1097/00007632-199105000-00011. PMID 1828912.
- ^ a b High risk pregnancy : management options. James, D. K. (David K.), Steer, Philip J. (4th ed.). St. Louis, MO: Saunders/Elsevier. 2011. ISBN 9781416059080. OCLC 727346377.
- ^ a b c Katonis, P.; Kampouroglou, A.; Aggelopoulos, A.; Kakavelakis, K.; Lykoudis, S.; Makrigiannakis, A.; Alpantaki, K. (July 1, 2011). "Pregnancy-related low back pain". Hippokratia. 15 (3): 205–210. ISSN 1108-4189.
- ^ a b c d e f Honorio Benzon, MD; James p. Rathmell, MD; Christopher l. Wu, MD; Dennis Turk, PhD; Charles e. Argoff, MD; Robert w Hurley, MD (2013-09-12). Practical management of pain. Benzon, Honorio T.,, Rathmell, James P.,, Wu, Christopher L.,, Turk, Dennis C.,, Argoff, Charles E.,, Hurley, Robert W. (Fifth ed.). Philadelphia, PA. ISBN 9780323083409. OCLC 859537559.
- ^ Conn's current therapy 2017. Bope, Edward T.,, Kellerman, Rick D.,, Preceded by: Conn, Howard F. (Howard Franklin), 1908-1982. Philadelphia: Elsevier. 2017. ISBN 9780323443203. OCLC 961064076.
External links[edit]
| Classification | |
|---|---|
| External resources |
- Back and spine at Curlie
- Handout on Health: Back Pain at National Institute of Arthritis and Musculoskeletal and Skin Diseases
- Qaseem, Amir; Wilt, Timothy J.; McLean, Robert M.; Forciea, Mary Ann (14 February 2017). "Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 166 (7): 514–530. doi:10.7326/M16-2367. PMID 28192789.
| Wikimedia Commons has media related to Back pain. |