Long QT syndrome
| Long QT syndrome | |
|---|---|
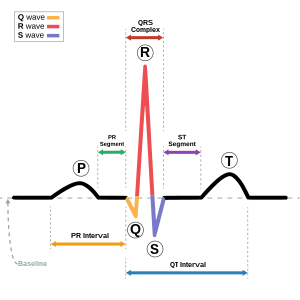 | |
| Drawing of a normal ECG tracing (sinus rhythm) with waves, segments, and intervals labeled. The QT interval is marked by the blue line at bottom. | |
| Specialty | Cardiology |
| Symptoms | Fainting, hearing loss[1] |
| Complications | Sudden death[1] |
| Causes | Genetic, certain medications, low blood potassium, low blood calcium, heart failure[2] |
| Risk factors | Family history of sudden death[3] |
| Diagnostic method | Electrocardiogram (EKG) together with clinical findings[4][3] |
| Differential diagnosis | Brugada syndrome, arrhythmogenic right ventricular dysplasia[3] |
| Treatment | Avoiding strenuous exercise, getting sufficient potassium, beta blockers, implantable cardiac defibrillator[5] |
| Frequency | ~ 1 in 7,000[5] |
| Deaths | ~3,500 a year (USA)[5] |
Long QT syndrome (LQTS) is a condition which affects repolarization of the heart after a heartbeat.[4] This results in an increased risk of an irregular heartbeat which can result in palpitations, fainting, drowning, or sudden death.[1] These episodes can be triggered by exercise or stress.[5] Other associated symptoms may include hearing loss.[1]
Long QT syndrome may be present at birth or develop later in life.[1] The inherited form may occur by itself or as part of larger genetic disorder.[1] Onset later in life may result from certain medications, low blood potassium, low blood calcium, or heart failure.[2] Medications that are implicated include certain antiarrhythmic, antibiotics, and antipsychotics.[2] Diagnosis is based on an electrocardiogram (EKG) finding a corrected QT interval of greater than 440 to 500 milliseconds together with clinical findings.[4][3]
Management may include avoiding strenuous exercise, getting sufficient potassium in the diet, the use of beta blockers, or an implantable cardiac defibrillator.[5] For people with LQTS who survive cardiac arrest and remain untreated, the risk of death within 15 years is greater than 50%.[6][5] With proper treatment this decreases to less than 1% over 20 years.[3]
Long QT syndrome is estimated to affect 1 in 7,000 people.[5] Females are affected more often than males.[5] Most people with the condition develop symptoms before they are 40 years old.[5] It is a relatively common cause of sudden death along with Brugada syndrome and arrhythmogenic right ventricular dysplasia.[3] In the United States it results in about 3,500 deaths a year.[5] The condition was first clearly described in 1957.[7]
Signs and symptoms[edit]
Many people with long QT syndrome have no signs or symptoms. Symptoms that do occur are generally caused by abnormal heart rhythms or arrhythmias, most commonly a form of ventricular tachycardia called Torsades de pointes. If the arrhythmia reverts to a normal rhythm by itself then the affected person may experience a faint known as syncope, which may be associated with seizures. However, if the arrhythmia continues, the affected person may experience a cardiac arrest leading to sudden death.[8]
The arrhythmias that lead to faints and sudden death are more likely to occur in response to specific circumstances, in part determined by which genetic variant is responsible for the condition. While arrhythmias can occur at any time, in some forms of LQTS arrhythmias are more commonly seen in response to exercise or mental stress (LQT1), in other forms following a sudden loud noise (LQT2) , and in some forms during sleep or immediately upon waking (LQT3).[8][9]
Some rare forms of long QT syndrome are associated with symptoms affecting other parts of the body. These include deafness in the Jervell and Lange-Nielsen form of the condition, and periodic paralysis in the Andersen-Tawil (LQT7) form.[10]
Risk for arrhythmias[edit]
While those with long QT syndrome have an increased risk of developing abnormal heart rhythms compared to those without the condition, the absolute risk of arrhythmias is very variable.[11] The strongest predictor of whether someone will develop torsades de pointes (TdP) is whether they have experienced spontaneous TdP or another form of cardiac arrest in the past.[12] Even if an arrhythmia has not been witnessed, a person with LQTS who has experienced syncope is also at higher risk, as syncope in these cases is frequently due to an undocumented self-terminating arrhythmia.[12]
In addition to a history of arrhythmias, the QT interval predicts risk. While some with LQTS will have QT intervals that are very prolonged, others will have only slight QT prolongation, or even a normal QT interval at rest (concealed LQTS). Those with the longest QT intervals are more likely to experience TdP, and a corrected QT interval of greater than 500 ms is thought to represent those at higher risk.[13] Despite this, even those with subtle QT prolongation or concealed LQTS still have some risk of arrhythmias.[8] Overall, every 10 ms increase in the corrected QT interval is associated with a 5% increase in arrhythmic risk.[11]
As the QT prolonging effects of both genetic variants and acquired causes of LQTS are additive, those with inherited LQTS are more likely to experience TdP if given QT prolonging drugs or develop electrolyte problems such as low potassium. Similarly, those taking QT prolonging medications are more likely to experience TdP if they have a genetic tendency to a prolonged QT interval, even it this tendency is concealed. [11] Arrhythmias occur more commonly in drug-induced LQTS if the medication in question has been rapidly given intravenously, or if high concentrations of the drug are present in the person's blood.[13] The risk of arrhythmias is also higher if the person receiving the drug has heart failure, is taking digitalis, or has recently been cardioverted from atrial fibrillation. [13] Other risk factors for developing torsades de pointes among those with LQTS include female sex, increasing age, pre-existing cardiovascular disease, and abnormal liver or kidney function.[14]
Causes[edit]
There are several subtypes of long QT syndrome. These can be broadly split into those caused by genetic mutations which those affected are born with, carry throughout their lives, and can pass on to their children (inherited or congenital long QT syndrome), and those caused by other factors which cannot be passed on and are often reversible (acquired long QT syndrome).
Acquired[edit]
Although Long QT syndrome is often a genetic condition, a prolonged QT interval associated with an increased risk of abnormal heart rhythms can also occur in people without a genetic abnormality, commonly due to a side effect of medications. Drug-induced QT prolongation is often a result of treatment by antiarrhythmic drugs such as amiodarone and sotalol, antibiotics such as erythomycin, or antihistamines such as terfenadine.[14] Other drugs which prolong the QT interval include some antipsychotics such as haloperidol and ziprasidone, and the antidepressant citalopram. [15] [13] Lists of medications associated with prolongation of the QT interval such as the QTdrugs database can be found online. [16]
Other causes of acquired LQTS include abnormally low levels of potassium (hypokalaemia) or magnesium (hypomagnesaemia) within the blood. This is can be exacerbated following a sudden reduction in the blood supply to the heart (myocardial infarction), low levels of thyroid hormone (hypothyroidism), and a slow heart rate (bradycardia). [17]
Anorexia nervosa has been associated with sudden death, possibly due to QT prolongation. The malnutrition seen in this condition can sometimes affect the blood concentration of salts such as potassium, potentially leading to acquired long QT syndrome, in turn causing sudden cardiac death. The malnutrition and associated changes in salt balance develop over a prolonged period of time, and rapid refeeding may further disturb the salt imbalances, increasing the risk of arrhythmias. Care must therefore be taken to monitor electrolyte levels to avoid the complications of refeeding syndrome.[18]
Factors which prolong the QT interval are additive, and genetic variants may make those who carry them more susceptible to drug-induced LQT. A combination of factors can cause a greater degree of QT prolongation than each factor alone. [17]
Genetics[edit]
Inherited, or congenital Long QT syndrome, is caused by genetic abnormalities. LQTS can arise from mutations in several genes, leading in some cases to quite different features.[19] The condition is most commonly inherited in an autosomal dominant manner, or rarely in an autosomal recessive fashion.[20] The autosomal recessive forms of LQTS tend to have a more severe phenotype. Genetic testing for LQTS is clinically available and may help to direct appropriate therapies.
Classification systems have been proposed to distinguish between subtypes of the condition. Modern classifications of inherited LQTS are based on identifying the underlying genetic variant that has caused the condition, giving rise to 16 subtypes of LQTS.[21] Alternatively, the classical descriptions of forms of inherited LQTS are based on clinical features and are named after those who first described the condition. The commonest of these, accounting for 99% of cases, is Romano-Ward syndrome (genetically LQT1-6 and LQT9-16), in which the electrical activity of the heart is affected without involvement of any other organs.[8] Other less commonly seen forms include Jervell and Lange-Nielsen syndrome, an autosomal recessive form of LQTS in which a combination of a prolonged QT interval and congenital deafness is seen; Anderson-Tawil syndrome (LQT7), which combines a prolonged QT interval with periodic paralysis and abnormalities of the face and skeleton; and Timothy syndrome (LQT8) which associates a prolonged QT interval with abnormalities in the structure of the heart and autism spectrum disorder.[10]
Genetic variants causing LQTS tend to prolong the duration of the ventricular action potential (APD), thus lengthening the QT interval. The most common causes of LQTS are mutations in the genes KCNQ1 (LQT1), KCNH2 (LQT2), and SCN5A (LQT3). [4] The following is a list of genes associated with LQTS:
| Type | OMIM | Gene | Notes |
| LQT1 | 192500 | KCNQ1 | Encodes the α-subunit of the slow delayed rectifier potassium channel KV7.1 carrying the potassium current IKs. [21] |
| LQT2 | 152427 | KCNH2 | Also known as hERG. Encodes the α-subunit of the rapid delayed rectifier potassium channel KV11.1 carrying the potassium current IKr. [21] |
| LQT3 | 603830 | SCN5A | Encodes the α-subunit of the cardiac sodium channel NaV1.5 carrying the sodium current INa. [21] |
| LQT4 | 600919 | ANK2 | Encodes Ankyrin B which anchors the ion channels in the cell. Disputed true association with QT prolongation. [21] |
| LQT5 | 176261 | KCNE1 | Encodes MinK, a potassium channel β-subunit. [21] |
| LQT6 | 603796 | KCNE2 | Encodes MiRP1, a potassium channel β-subunit. [21] |
| LQT7 | 170390 | KCNJ2 | Encodes inward rectifying potassium current Kir2.2 carrying the potassium current IK1. Causes Andersen-Tawil syndrome. [21] |
| LQT8 | 601005 | CACNA1c | Encodes the α-subunit CaV1.2 of the calcium channel Cav1.2 carrying the calcium current ICa(L). Causes Timothy syndrome. [21] |
| LQT9 | 611818 | CAV3 | Encodes Caveolin-3, responsible for forming membrane pouches known as caveolae. Mutations in this gene may increase the late sodium current INa. [21] |
| LQT10 | 611819 | SCN4B | Encodes the β4-subunit of the cardiac sodium channel. [21] |
| LQT11 | 611820 | AKAP9 | Encodes A-kinase associated protein which interacts with KV7.1. [21] |
| LQT12 | 601017 | SNTA1 | Encodes syntrophin-α1. Mutations in this gene may increase the late sodium current INa. [21] |
| LQT13 | 600734 | KCNJ5 | Also known as GIRK4, encodes G protein-sensitive inwardly rectifying potassium channels (Kir3.4) which carry the potassium current IK(ACh). [21] |
| LQT14 | 616247 | CALM1 | Encodes calmodulin-1, a calcium-binding messenger protein that interacts with the calcium current ICa(L). [21] |
| LQT15 | 616249 | CALM2 | Encodes calmodulin-2, a calcium-binding messenger protein that interacts with the calcium current ICa(L). [21] |
| LQT16 | 114183 | CALM3 | Encodes calmodulin-3, a calcium-binding messenger protein that interacts with the calcium current ICa(L). [21] |
- LQT1
LQT1 is the most common type of long QT syndrome,[4] making up about 30 to 35% of all cases. The LQT1 gene is KCNQ1, which has been isolated to chromosome 11p15.5. KCNQ1 codes for the voltage-gated potassium channel KvLQT1 that is highly expressed in the heart. The product of the KCNQ1 gene is thought to produce an alpha subunit that interacts with other proteins (in particular, the minK beta subunit) to create the IKs ion channel, which is responsible for the delayed potassium rectifier current of the cardiac action potential.
Mutations to KCNQ1 can be inherited in an autosomal dominant or an autosomal recessive pattern in the same family. In the autosomal recessive mutation of this gene, homozygous mutations lead to severe prolongation of the QT interval (due to near-complete loss of the IKs ion channel), and are associated with increased risk of ventricular arrhythmias and congenital deafness. This variant of LQT1 is known as the Jervell and Lange-Nielsen syndrome.[22] Furthermore, LQT1 patients also have an endocrine phenotype. During a glucose load, LQT1 patients respond with an exaggerated insulin secretion followed by a temporary insulin resistance. When the resistance diminishes, LQT1 patients are at risk for hypoglycaemia.[23]
Most individuals with LQT1 show paradoxical prolongation of the QT interval with infusion of epinephrine. This can also unmark latent carriers of the LQT1 gene. Many missense mutations of the LQT1 gene have been identified. These are often associated with a high frequency of syncopes, but less sudden death than LQT2.
- LQT2
The LQT2 type is the second-most common gene location in long QT syndrome, making up about 25 to 30% of all cases. This form of long QT syndrome most likely involves mutations of the 'human ether-a-go-go related gene' (hERG) on chromosome 7. The hERG gene (also known as KCNH2) is part of the rapid component of the potassium rectifying current (IKr). (The IKr current is mainly responsible for the termination of the cardiac action potential, and therefore the length of the QT interval.) The normally functioning hERG gene allows protection against early after depolarizations.[24]
Most drugs that cause long QT syndrome do so by blocking the IKr current via the hERG gene. These include erythromycin, terfenadine, and ketoconazole. The hERG channel is very sensitive to unintended drug binding due to two aromatic amino acids, the tyrosine at position 652 and the phenylalanine at position 656. These amino acid residues are poised so a drug binding to them blocks the channel from conducting current. Other potassium channels do not have these residues in these positions, so are, therefore, not as prone to blockage.
- LQT3
The LQT3 type of long QT syndrome involves mutation of the gene that encodes the alpha subunit of the Na+ ion channel. This gene is located on chromosome 3p21-24, and is known as SCN5A (also hH1 and NaV1.5). The mutations involved in LQT3 slow the inactivation of the Na+ channel, resulting in prolongation of the Na+ influx during depolarization. However, the mutant sodium channels inactivate more quickly, and may open repetitively during the action potential.
A large number of mutations have been characterized as leading to or predisposing to LQT3. Calcium has been suggested as a regulator of SCN5A protein, and the effects of calcium on SCN5A may begin to explain the mechanism by which some these mutations cause LQT3. Furthermore, mutations in SCN5A can cause Brugada syndrome, cardiac conduction disease, and dilated cardiomyopathy. In rare situations, some affected individuals can have combinations of these diseases.
- LQT5
LQT5 is an autosomal-recessive, relatively uncommon form of LQTS. It involves mutations in the gene KCNE1, which encodes for the potassium channel beta subunit MinK. In its rare homozygous forms, it can lead to Jervell and Lange-Nielsen syndrome.
- LQT6
LQT6 is an autosomal-dominant, relatively uncommon form of LQTS. It involves mutations in the gene KCNE2, which encodes for the potassium channel beta subunit MiRP1, constituting part of the IKr repolarizing K+ current.
- LQT7
Andersen-Tawil syndrome is an autosomal-dominant form of LQTS associated with skeletal deformities. It involves mutation in the gene KCNJ2, which encodes for the potassium channel protein Kir 2.1. The syndrome is characterized by LQTS with ventricular arrhythmias, periodic paralysis, and skeletal developmental abnormalities such as clinodactyly, low-set ears, and micrognathia. The manifestations are highly variable.[25]
- LQT8
Timothy syndrome is due to mutations in the calcium channel Cav1.2 encoded by the gene CACNA1c. Since the calcium channel Cav1.2 is abundant in many tissues, patients with Timothy syndrome have many clinical manifestations, including other congenital heart disease, autism, immune deficiency and complex syndactyly.[26]
- LQT9
This newly discovered variant is caused by mutations in the membrane structural protein, caveolin-3. Caveolins form specific membrane domains called caveolae in which, among others, the NaV1.5 voltage-gated sodium channel sits. Similar to LQT3, these particular mutations increase so-called 'late' sodium current, which impairs cellular repolarization.
- LQT10
This novel susceptibility gene for LQT is SCN4B encoding the protein NaVβ4, an auxiliary subunit to the pore-forming NaV1.5 (gene: SCN5A) subunit of the voltage-gated sodium channel of the heart. The mutation leads to a positive shift in inactivation of the sodium current, thus increasing sodium current. Only one mutation in one patient has so far been found.
- LQT13
GIRK4 is involved in the parasympathetic modulation of the heart. Clinically, the patients are characterized by only modest QT prolongation, but an increased propensity for atrial arrhythmias.[27]
- LQT14
LQT14 is caused by heterozygous mutations in the CALM1 (Calmodulin 1) gene (114180) on chromosome 14q32.
- LQT15
LQT15 is caused by heterozygous mutations in the CALM2 (Calmodulin 2) gene (114182) on chromosome 2p21.
- LQT16
LQT16 is caused by heterozygous mutations in the CALM3 (Calmodulin 3) gene (114183) on chromosome 19q13.
Pathophysiology[edit]
LQTS is classified a form of channelopathy.
All forms of LQTS involve an abnormal repolarization of the heart, which causes differences in the refractory period of the heart muscle cells (myocytes). After-depolarizations (which occur more commonly in LQTS) can be propagated to neighboring cells due to the differences in the refractory periods, leading to re-entrant ventricular arrhythmias.
The so-called early after-depolarizations (EADs) seen in LQTS are believed to be due to reopening of L-type calcium channels during the plateau phase of the cardiac action potential. Since adrenergic stimulation can increase the activity of these channels, this is an explanation for why the risk of sudden death in individuals with LQTS is increased during increased adrenergic states (i.e., exercise, excitement), especially since repolarization is impaired. Normally during adrenergic states, repolarizing currents also are enhanced to shorten the action potential. In the absence of this shortening and the presence of increased L-type calcium current, EADs may arise.
The so-called delayed after-depolarizations are thought to be due to an increased Ca2+ filling of the sarcoplasmic reticulum. This overload may cause spontaneous Ca2+ release during repolarization, causing the released Ca2+ to exit the cell through the 3Na+/Ca2+-exchanger, which results in a net depolarizing current.
Diagnosis[edit]
The diagnosis of LQTS is not easy since 2.5% of the healthy population has prolonged QT interval, and 10–15% of LQTS patients have a normal QT interval.[28] A commonly used criterion to diagnose LQTS is the LQTS "diagnostic score",[29] calculated by assigning different points to various criteria (listed below). With four or more points, the probability is high for LQTS; with one point or less, the probability is low.[4] A score of two or three points indicates intermediate probability.[4]
- QTc (Defined as QT interval / square root of RR interval)
- ≥ 480 ms - 3 points
- 460-470 ms - 2 points
- 450 ms and male gender - 1 point
- Torsades de pointes ventricular tachycardia - 2 points
- T wave alternans - 1 point
- Notched T wave in at least 3 leads - 1 point
- Low heart rate for age (children) - 0.5 points
- Syncope (one cannot receive points both for syncope and torsades de pointes)
- With stress - 2 points
- Without stress - 1 point
- Congenital deafness - 0.5 points
- Family history (the same family member cannot be counted for LQTS and sudden death)
- Other family members with definite LQTS - 1 point
- Sudden death in immediate family members (before age 30) - 0.5 points
Treatment[edit]
Those diagnosed with LQTS are usually advised to avoid drugs that would prolong the QT interval further or lower the threshold for TDP.[30] In addition to this, two intervention options are known for individuals with LQTS: arrhythmia prevention and arrhythmia termination.
Arrhythmia prevention[edit]
Arrhythmia suppression involves the use of medications or surgical procedures that attack the underlying cause of the arrhythmias associated with LQTS. Since the cause of arrhythmias in LQTS is EADs, and they are increased in states of adrenergic stimulation, steps can be taken to blunt adrenergic stimulation in these individuals. These include administration of beta receptor blocking agents, which decreases the risk of stress-induced arrhythmias. Beta blockers are an effective treatment for LQTS caused by LQT1 and LQT2.[4]
Genotype and QT interval duration are independent predictors of recurrence of life-threatening events during beta-blocker therapy. To be specific, the presence of QTc >500 ms and LQT2 and LQT3 genotype are associated with the highest incidence of recurrence. In these patients, primary prevention with use of implantable cardioverter-defibrillators can be considered.[4]
- Potassium supplementation: If the potassium content in the blood rises, the action potential shortens, so increasing potassium concentration could minimize the occurrence of arrhythmias. It should work best in LQT2, since the hERG channel is especially sensitive to potassium concentration, but the use is experimental and not evidence-based.
- Mexiletine, a sodium channel blocker: In LQT3, the sodium channel does not close properly. Mexiletine closes these channels and is believed to be usable when other therapies fail. Theoretically, mexiletine could be useful for people with this form of LQTS, but the medication is currently under study for this application and its use is not currently recommended.[4]
- Amputation of the cervical sympathetic chain (left stellectomy). This therapy is typically reserved for LQTS caused by JLNS,[4] but may be used as an add-on therapy to beta blockers in certain cases. In most cases, modern therapy favors ICD implantation if beta blocker therapy fails.
Arrhythmia termination[edit]
Arrhythmia termination involves stopping a life-threatening arrhythmia once it has already occurred. One effective form of arrhythmia termination in individuals with LQTS is placement of an implantable cardioverter-defibrillator (ICD). Also, external defibrillation can be used to restore sinus rhythm. ICDs are commonly used in patients with fainting episodes despite beta blocker therapy, and in patients having experienced a cardiac arrest.
With better knowledge of the genetics underlying LQTS, more precise treatments hopefully will become available.[31]
Outcomes[edit]
For people who experience cardiac arrest or fainting caused by LQTS and who are untreated, the risk of death within 15 years is around 50%.[6] With careful treatment this decreases to less than 1% over 20 years.[3]Those who exhibit symptoms before the age of 18 are more likely to experience a cardiac arrest.[32][33]
Epidemiology[edit]
Inherited LQTS is estimated to affect between one in 2,500 and 7,000 people.[4]
History[edit]
The first documented case of LQTS was described in Leipzig by Meissner in 1856, when a deaf girl died after her teacher yelled at her. When the parents were notified of her death, they reported that her older brother, who also was deaf, died after a terrible fright.[34] This was several decades before the ECG was invented, but is likely the first described case of Jervell and Lange-Nielsen syndrome. In 1957, the first case documented by ECG was described by Anton Jervell and Fred Lange-Nielsen, working in Tønsberg, Norway.[35] Italian pediatrician Cesarino Romano, in 1963,[36] and Irish pediatrician Owen Conor Ward, in 1964,[37] separately described the more common variant of LQTS with normal hearing, later called Romano-Ward syndrome. The establishment of the International Long-QT Syndrome Registry in 1979 allowed numerous pedigrees to be evaluated in a comprehensive manner. This helped in detecting many of the numerous genes involved.[38]
See also[edit]
References[edit]
- ^ a b c d e f "Long QT syndrome". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. 2017. Retrieved 14 December 2017.
- ^ a b c Morita H, Wu J, Zipes DP (August 2008). "The QT syndromes: long and short". Lancet. 372 (9640): 750–63. doi:10.1016/S0140-6736(08)61307-0. PMID 18761222.
- ^ a b c d e f g Ferri, Fred F. (2016). Ferri's Clinical Advisor 2017 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 736. ISBN 9780323448383.
- ^ a b c d e f g h i j k l Levine E, Rosero SZ, Budzikowski AS, Moss AJ, Zareba W, Daubert JP (August 2008). "Congenital long QT syndrome: considerations for primary care physicians". Cleveland Clinic Journal of Medicine. 75 (8): 591–600. PMID 18756841.
- ^ a b c d e f g h i j "Long QT Syndrome". NHLBI, NIH. Retrieved 14 December 2017.
- ^ a b Ackerman MJ, Priori SG, Dubin AM, Kowey P, Linker NJ, Slotwiner D, Triedman J, Van Hare GF, Gold MR (January 2017). "Beta-blocker therapy for long QT syndrome and catecholaminergic polymorphic ventricular tachycardia: Are all beta-blockers equivalent?". Heart Rhythm. 14 (1): e41–e44. doi:10.1016/j.hrthm.2016.09.012. PMID 27659101.
Among patients who have experienced a LQTS-triggered cardiac event (arrhythmic syncope, arrhythmic syncope followed by seizures, or aborted cardiac arrest), the untreated natural history is grim, with >50% mortality at 15 years.

- ^ Vincent J, Abraham E, Kochanek P, Moore FA, Fink MP (2011). Textbook of Critical Care E-Book. Elsevier Health Sciences. p. 578. ISBN 978-1437715682.
- ^ a b c d Tester DJ, Schwartz PJ, Ackerman MJ (2013). Gussak I, Antzelevitch C, eds. Congenital Long QT Syndrome. Electrical Diseases of the Heart: Volume 1: Basic Foundations and Primary Electrical Diseases. Springer London. pp. 439–468. doi:10.1007/978-1-4471-4881-4_27. ISBN 9781447148814.
|access-date=requires|url=(help) - ^ Nakajima T, Kaneko Y, Kurabayashi M (2015). "Unveiling specific triggers and precipitating factors for fatal cardiac events in inherited arrhythmia syndromes". Circulation Journal. 79 (6): 1185–92. doi:10.1253/circj.CJ-15-0322. PMID 25925977.
- ^ a b Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. (November 2015). "2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC)". Europace. 17 (11): 1601–87. doi:10.1093/europace/euv319. PMID 26318695.
- ^ a b c Trinkley, Katy E.; Page, Robert Lee; Lien, Hoang; Yamanouye, Kevin; Tisdale, James E. (December 2013). "QT interval prolongation and the risk of torsades de pointes: essentials for clinicians". Current Medical Research and Opinion. 29 (12): 1719–1726. doi:10.1185/03007995.2013.840568. ISSN 1473-4877. PMID 24020938.
- ^ a b Barsheshet, Alon; Dotsenko, Olena; Goldenberg, Ilan (November 2013). "Genotype-specific risk stratification and management of patients with long QT syndrome". Annals of Noninvasive Electrocardiology: The Official Journal of the International Society for Holter and Noninvasive Electrocardiology, Inc. 18 (6): 499–509. doi:10.1111/anec.12117. ISSN 1542-474X. PMID 24206565.
- ^ a b c d Roden, Dan M. (2004-03-04). "Drug-induced prolongation of the QT interval". The New England Journal of Medicine. 350 (10): 1013–1022. doi:10.1056/NEJMra032426. ISSN 1533-4406. PMID 14999113.
- ^ a b Thomson, Clare; Wright, Paul (2014-10-15). "Long QT syndrome". The Pharmaceutical Journal. 293 (7833). Retrieved 18 October 2014.
- ^ Beach, Scott R.; Celano, Christopher M.; Noseworthy, Peter A.; Januzzi, James L.; Huffman, Jeff C. (January 2013). "QTc prolongation, torsades de pointes, and psychotropic medications". Psychosomatics. 54 (1): 1–13. doi:10.1016/j.psym.2012.11.001. ISSN 1545-7206. PMID 23295003.
- ^ Woosley, Raymond L.; Black, Kristin; Heise, C. William; Romero, Klaus (February 2018). "CredibleMeds.org: What does it offer?". Trends in Cardiovascular Medicine. 28 (2): 94–99. doi:10.1016/j.tcm.2017.07.010. ISSN 1873-2615. PMID 28801207.
- ^ a b El-Sherif N, Turitto G, Boutjdir M (April 2018). "Acquired long QT syndrome and torsade de pointes". Pacing and Clinical Electrophysiology. 41 (4): 414–421. doi:10.1111/pace.13296. PMID 29405316.
- ^ Jáuregui-Garrido B, Jáuregui-Lobera I (February 2012). "Sudden death in eating disorders". Vascular Health and Risk Management. 8: 91–8. doi:10.2147/VHRM.S28652. PMC 3292410. PMID 22393299.
- ^ Hedley PL, Jørgensen P, Schlamowitz S, Wangari R, Moolman-Smook J, Brink PA, Kanters JK, Corfield VA, Christiansen M (November 2009). "The genetic basis of long QT and short QT syndromes: a mutation update". Human Mutation. 30 (11): 1486–511. doi:10.1002/humu.21106. PMID 19862833.
- ^ Goldman 2011, pp. 185
- ^ a b c d e f g h i j k l m n o p q Giudicessi JR, Wilde AA, Ackerman MJ (October 2018). "The genetic architecture of long QT syndrome: A critical reappraisal". Trends in Cardiovascular Medicine. 28 (7): 453–464. doi:10.1016/j.tcm.2018.03.003. PMID 29661707.
- ^ Schwartz PJ, Spazzolini C, Crotti L, Bathen J, Amlie JP, Timothy K, Shkolnikova M, Berul CI, Bitner-Glindzicz M, Toivonen L, Horie M, Schulze-Bahr E, Denjoy I (February 2006). "The Jervell and Lange-Nielsen syndrome: natural history, molecular basis, and clinical outcome". Circulation. 113 (6): 783–90. doi:10.1161/CIRCULATIONAHA.105.592899. PMID 16461811.
- ^ Torekov SS, Iepsen E, Christiansen M, Linneberg A, Pedersen O, Holst JJ, Kanters JK, Hansen T (April 2014). "KCNQ1 long QT syndrome patients have hyperinsulinemia and symptomatic hypoglycemia". Diabetes. 63 (4): 1315–25. doi:10.2337/db13-1454. PMID 24357532.
- ^ Shinnawi R, Gepstein L (September 2014). "iPCS Cell Modeling of Inherited Cardiac Arrhythmias". Current Treatment Options in Cardiovascular Medicine. 16 (9): 331. doi:10.1007/s11936-014-0331-4. PMID 25080030.
- ^ Tristani-Firouzi M, Jensen JL, Donaldson MR, Sansone V, Meola G, Hahn A, Bendahhou S, Kwiecinski H, Fidzianska A, Plaster N, Fu YH, Ptacek LJ, Tawil R (August 2002). "Functional and clinical characterization of KCNJ2 mutations associated with LQT7 (Andersen syndrome)". The Journal of Clinical Investigation. 110 (3): 381–8. doi:10.1172/JCI15183. PMC 151085. PMID 12163457.
- ^ Shah DP, Baez-Escudero JL, Weisberg IL, Beshai JF, Burke MC (March 2012). "Ranolazine safely decreases ventricular and atrial fibrillation in Timothy syndrome (LQT8)". Pacing and Clinical Electrophysiology. 35 (3): e62–4. doi:10.1111/j.1540-8159.2010.02913.x. PMID 20883512.
- ^ Wang F, Liu J, Hong L, Liang B, Graff C, Yang Y, Christiansen M, Olesen SP, Zhang L, Kanters JK (October 2013). "The phenotype characteristics of type 13 long QT syndrome with mutation in KCNJ5 (Kir3.4-G387R)". Heart Rhythm. 10 (10): 1500–6. doi:10.1016/j.hrthm.2013.07.022. PMID 23872692.
- ^ Moric-Janiszewska E, Markiewicz-Łoskot G, Łoskot M, Weglarz L, Hollek A, Szydłowski L (September 2007). "Challenges of diagnosis of long-QT syndrome in children". Pacing and Clinical Electrophysiology. 30 (9): 1168–70. doi:10.1111/j.1540-8159.2007.00832.x. PMID 17725765.
- ^ Schwartz PJ, Moss AJ, Vincent GM, Crampton RS (August 1993). "Diagnostic criteria for the long QT syndrome. An update". Circulation. 88 (2): 782–4. doi:10.1161/01.CIR.88.2.782. PMID 8339437.
- ^ "QT Drug List by Risk Groups". Arizona Center for Education and Research on Therapeutics. Archived from the original on 2010-12-24. Retrieved 2010-07-04.
- ^ Compton SJ, Lux RL, Ramsey MR, Strelich KR, Sanguinetti MC, Green LS, Keating MT, Mason JW (September 1996). "Genetically defined therapy of inherited long-QT syndrome. Correction of abnormal repolarization by potassium". Circulation. 94 (5): 1018–22. doi:10.1161/01.CIR.94.5.1018. PMID 8790040.
- ^ Giudicessi JR, Ackerman MJ (October 2013). "Genotype- and phenotype-guided management of congenital long QT syndrome". Current Problems in Cardiology. 38 (10): 417–55. doi:10.1016/j.cpcardiol.2013.08.001. PMC 3940076. PMID 24093767.
- ^ "Genotype risk relationship".
- ^ Tranebjaerg L, Bathen J, Tyson J, Bitner-Glindzicz M (September 1999). "Jervell and Lange-Nielsen syndrome: a Norwegian perspective". American Journal of Medical Genetics. 89 (3): 137–46. doi:10.1002/(SICI)1096-8628(19990924)89:3<137::AID-AJMG4>3.0.CO;2-C. PMID 10704188.
- ^ Jervell A, Lange-Nielsen F (July 1957). "Congenital deaf-mutism, functional heart disease with prolongation of the Q-T interval and sudden death". American Heart Journal. 54 (1): 59–68. doi:10.1016/0002-8703(57)90079-0. PMID 13435203.
- ^ Romano C, Gemme G, Pongiglione R (September 1963). "[RARE CARDIAC ARRYTHMIAS OF THE PEDIATRIC AGE. II. SYNCOPAL ATTACKS DUE TO PAROXYSMAL VENTRICULAR FIBRILLATION. (PRESENTATION OF 1ST CASE IN ITALIAN PEDIATRIC LITERATURE)]". La Clinica Pediatrica (in Italian). 45: 656–83. PMID 14158288.
- ^ Ward OC (April 1964). "A NEW FAMILIAL CARDIAC SYNDROME IN CHILDREN". Journal of the Irish Medical Association. 54: 103–6. PMID 14136838.
- ^ Moss AJ, Schwartz PJ (March 2005). "25th anniversary of the International Long-QT Syndrome Registry: an ongoing quest to uncover the secrets of long-QT syndrome". Circulation. 111 (9): 1199–201. doi:10.1161/01.CIR.0000157069.91834.DA. PMID 15753228.
- Notes
- Goldman, Lee (2011). Goldman's Cecil Medicine (24th ed.). Philadelphia: Elsevier Saunders. p. 1196. ISBN 978-1437727883.
External links[edit]
| Classification | |
|---|---|
| External resources |
- Long QT syndrome at Curlie
- CredibleMeds.org, contains a list of drugs that prolong the QT interval
.jpg/290px-De-Acquired_longQT_(CardioNetworks_ECGpedia).jpg)